
Man tied to Lebanon school lockdowns pleads not guilty to charges
LEBANON — A Vershire man has pleaded not guilty to criminal charges stemming from an incident that provoked a lockdown at Lebanon High School and Hanover Street School in March when he allegedly approached the school campus with loaded weapons in his...

New Mascoma equestrian team has early success
WEST CANAAN — The group might be small with only four athletes, but so far the success of Mascoma Valley Regional High School’s newest team has been large.The newly formed Mascoma equestrian team — Molly Gray, Aubrey Meyveagaci, Abby Waugh and Rainah...
Most Read
 At Dartmouth, hundreds protest ongoing war in Gaza and express support for academic freedom
At Dartmouth, hundreds protest ongoing war in Gaza and express support for academic freedom
 Herd departs Hartford’s last remaining dairy farm
Herd departs Hartford’s last remaining dairy farm
 Lebanon moves forward with plans for employee housing
Lebanon moves forward with plans for employee housing
 Colby-Sawyer president announces plan to depart
Colby-Sawyer president announces plan to depart
 Windsor man who failed to show up for trial arrested in Hartland
Windsor man who failed to show up for trial arrested in Hartland
Editors Picks
 Herd departs Hartford’s last remaining dairy farm
Herd departs Hartford’s last remaining dairy farm
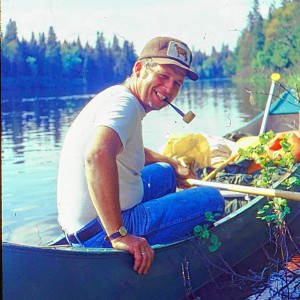 A Life: Richard Fabrizio ‘was not getting rich but was doing something that made him happy’
A Life: Richard Fabrizio ‘was not getting rich but was doing something that made him happy’
 Kenyon: What makes Dartmouth different?
Kenyon: What makes Dartmouth different?
 Publisher’s note: Valley News launches updated online app
Publisher’s note: Valley News launches updated online app
Sports

Local Roundup: Lebanon wins big over Bow in boys tennis
Editor’s note: To have your team’s results included in the Local Roundup, visit https://www.vnews.com/submit-a-score.Boys Tennis Lebanon 8, Bow 1 Key players: Lebanon — Nolan Arado, Will Katz Highlights: It was Senior Night, and the seniors held...
 Lebanon has chances but still can’t solve Hanover baseball mystery
Lebanon has chances but still can’t solve Hanover baseball mystery
 Volunteers work to repair Upper Valley trails damaged by storms
Volunteers work to repair Upper Valley trails damaged by storms
 Local Roundup: Hanover hangs on for 11-9 softball win over Lebanon
Local Roundup: Hanover hangs on for 11-9 softball win over Lebanon
Opinion

Editorial: Chris Sununu’s moral vacuum
New Hampshire Gov. Chris Sununu’s conversion from “Never Trump” to “Ever Trump” occurred not on the road to Damascus but on the Republican Party’s road to perdition.On ABC News last Sunday, Sununu affirmed his intention to support Donald Trump for...
 Editorial: Gambling tarnishes America’s sporting life
Editorial: Gambling tarnishes America’s sporting life
 By the Way: A white nationalist’s many mistruths
By the Way: A white nationalist’s many mistruths
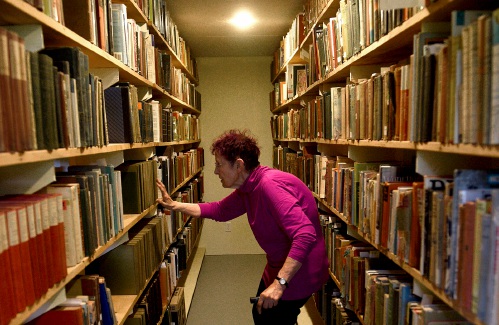 Column: The age-old question of what to read
Column: The age-old question of what to read
 Editorial: Transparency wins in NH Supreme Court ruling
Editorial: Transparency wins in NH Supreme Court ruling

Photos

Spring cleanup in Lebanon
 Drawn to dragons
Drawn to dragons
 Clear and free in Hartford
Clear and free in Hartford
 Ramping up their foraging
Ramping up their foraging
 Roadside assist in Bethel
Roadside assist in Bethel
Arts & Life

Bald eagles are back, but great blue herons paid the price
After years of absence, the most patriotic bird in the sky returned to Vermont — but it might’ve come at another’s expense.Vermont finally took the bald eagle off of its endangered species list in 2022 following years of reintroduction efforts...
 JAG Productions announces closure, citing ‘crisis facing the arts’
JAG Productions announces closure, citing ‘crisis facing the arts’
 How a hurricane and a cardinal launched a UVM professor on a new career path
How a hurricane and a cardinal launched a UVM professor on a new career path
Obituaries
 Kevin Currier
Kevin Currier
Topsham, VT - Kevin Charles Currier died unexpectedly at his home in Topsham, VT on April 13, 2024 at the age of 62. Our beloved Cubby, Bub or Bubby, as he was fondly called by his family and friends, was born on May 22, 1961 to Charle... remainder of obit for Kevin Currier
 Ann Young
Ann Young
Rye, NH - Ann Eastman Young was born in Hanover, New Hampshire, in the wee hours of April 21, 1958. She remained a morning person for the rest of her life, embracing sunrises from New Hampshire to Florida, California and beyond. She gre... remainder of obit for Ann Young
 Garry V. Hosford
Garry V. Hosford
St. Johnsbury, VT - Garry V. Hosford, 66, died on Sunday, April 28, 2024, at the St. Johnsbury Health and Rehab Center. He was born in Windsor, Vermont on December 29, 1957, the third child of Lawrence and Harriett (Manning) Hosford and... remainder of obit for Garry V. Hosford
 Michael D. Skinner
Michael D. Skinner
Lebanon, NH - Michael D. Skinner, of Lebanon, NH and Tenant's Harbor, ME, passed away peacefully on April 27, 2024, surrounded by loved ones. Mike was many things to many people, but most importantly he was a loving husband, devoted fat... remainder of obit for Michael D. Skinner


 Oxbow softball at dynastic, dominant best
Oxbow softball at dynastic, dominant best
 Local Roundup: Hanover, Lebanon girls tennis teams are undefeated
Local Roundup: Hanover, Lebanon girls tennis teams are undefeated
 Dartmouth graduate student-workers go on strike
Dartmouth graduate student-workers go on strike
 On the trail: NH Democrats quietly hold second presidential primary
On the trail: NH Democrats quietly hold second presidential primary
 Search underway for hiker in NH last seen two weeks ago
Search underway for hiker in NH last seen two weeks ago

 Out & About: Newport art center’s exhibition celebrates homes of all varieties
Out & About: Newport art center’s exhibition celebrates homes of all varieties
