Editorial: Are we now receiving better care?
| Published: 01-22-2023 3:41 PM |
When the organization now known as Dartmouth Health first began swallowing up smaller hospitals and medical practices in the Upper Valley and in the wider region, it articulated a vision of a unified system in which patients would receive “the right care, at the right time, in the right place.”
As time went on, this vision was fleshed out to include primary care physicians who would treat routine illnesses, help patients manage chronic conditions, and coordinate care while serving as advocates when their patients required treatment by specialists. The severely ill who required complicated and specialized treatment in a hospital would go to Dartmouth Hitchcock Medical Center, while those less severely sick would be treated at the smaller, affiliated hospitals. All this would be accomplished seamlessly with the aid of a comprehensive, universal health records system.
Not only that, a larger population base would provide the system with the market power to bargain with insurers and suppliers, resulting in efficiencies across the board. And it would be the key to implementing the payment system reforms pioneered by research on health care delivery conducted at The Dartmouth Institute.
Ten years later, this vision appears to us to be like nothing so much as a mirage in the desert, receding farther with each step taken forward.
This judgment is harsh, to be sure. It is not intended to reflect on the best efforts of thousands of faithful DH employees who skillfully treat multitudes of patients under often trying conditions.
Nor do we suggest that the original vision outlined for the health system was flawed. In fact, it constituted a highly desirable outcome. But at this point, the question has to be asked how realistic it was. Or put another way, are DH patients more satisfied with their health care now than they were a decade ago?
As our colleague Nora Doyle-Burr reported recently, the system’s flagship hospital, the 396-bed Dartmouth Hitchcock Medical Center in Lebanon, has been operating over capacity for several weeks as respiratory viruses surge and acute staff shortages persist. A lack of beds at facilities that provide lower levels of care means that DHMC has to board patients ready for discharge in its emergency department and perioperative areas, forcing other patients to experience delays in scheduling appointments and procedures. Meanwhile, smaller hospitals have to scramble to find other accommodations for their patients who require the higher level of care available at the academic medical center.
Moreover, a lack of primary care physicians in the system has resulted in DH “pausing” the acceptance of new primary care patients in some locations for nearly a year. Waiting times for existing patients to make appointments with their primary care physicians range up to six months. And when those patients do get sick with routine illnesses, they are diverted to walk-in clinics where they often wait for hours to see a physician assistant, or to stand-alone urgent care centers.
Article continues after...
Yesterday's Most Read Articles
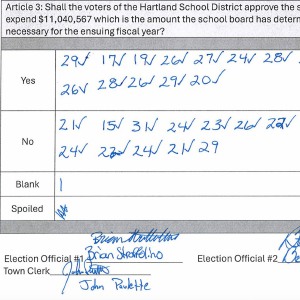 Hartland voters successfully petition for school budget revote
Hartland voters successfully petition for school budget revote
 JAG Productions announces closure, citing ‘crisis facing the arts’
JAG Productions announces closure, citing ‘crisis facing the arts’
 Hanover’s Perreard may soon capture the attention of collegiate coaches in two athletic pursuits
Hanover’s Perreard may soon capture the attention of collegiate coaches in two athletic pursuits
In the bigger picture, it is hard to see much progress in the transition from a fee-for-service payment system to one in which health systems are financially rewarded for how effectively they keep their populations well, although DH is a participant in one such experiment in Vermont. And the effect of consolidation on prices paid by patients and insurers remains opaque.
Of course, these perceived shortcomings must be viewed in the context of problems besetting health care across the region and the nation, in particular the shortage of health care workers. And the COVID-19 pandemic certainly placed unprecedented stress on virtually all health care systems. But DH is the system we have here in the Upper Valley, where health care choice and competition are now extremely limited, so our attention is naturally focused on that organization.
In addition to DHMC, DH now encompasses Mt. Ascutney, New London and Alice Peck Day hospitals, Cheshire Medical Center, and the Visiting Nurse and Hospice for Vermont and New Hampshire. Additional affiliations are pending with Valley Regional Hospital in Claremont and Southwestern Vermont Medical Center in Bennington. DH has also unsuccessfully chased potential partners in the lucrative southern New Hampshire market.
At this point, there’s no going back on consolidation of the DH system. But it is perhaps time for its leaders to ask whether smaller, decentralized units that can change course more nimbly in a rapidly changing health care environment might better serve patients, and perhaps aid in recruiting clinicians who seek more scope for autonomous decision-making in providing the right care, at the right time, in the right place.

 Editorial: Chris Sununu’s moral vacuum
Editorial: Chris Sununu’s moral vacuum Editorial: Gambling tarnishes America’s sporting life
Editorial: Gambling tarnishes America’s sporting life By the Way: A white nationalist’s many mistruths
By the Way: A white nationalist’s many mistruths Column: The age-old question of what to read
Column: The age-old question of what to read
