End of Medicaid’s pandemic rules will force many in NH, Vt. to seek new coverage
| Published: 02-01-2023 6:33 PM |
WHITE RIVER JUNCTION — Tens of thousands of residents in Vermont and New Hampshire could lose their health care coverage under Medicaid as the eligibility requirements return to pre-pandemic rules.
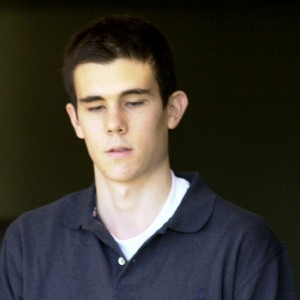
That includes Griffin Shumway, a 33-year-old middle school teacher who lives in White River Junction, who says he’s anxious about the change, which will be implemented gradually and give those whose income qualifies a chance to continue their coverage. Shumway, who was laid off from a job at Dartmouth College in 2020 and subsequently earned a teaching certificate at the Upper Valley Educators Institute, said he is concerned that losing his Medicaid coverage will make it harder to get the care he needs at an affordable price.
His school-sponsored coverage through Blue Cross Blue Shield includes a $4,000 deductible, which Shumway, who earns about $44,000 annually, said is like not having coverage.
It’s “there in an emergency I guess,” he said in a phone interview.
Medicaid covered Shumway’s visit to the emergency department following a dog bite, which he estimates could have cost as much as $1,000 without that coverage. In addition, Medicaid has covered an eye test he is supposed to get annually due to an eye injury he suffered while in college. Without Medicaid, he expects he’ll be forced to pay for the $300 test himself.
“I can barely afford my rent right now,” said Shumway, who along with his partner pays $1,750 monthly for a two-bedroom in White River Junction.
Under pandemic-era rules, people like Shumway who lost their jobs during the public health emergency as well as others on Medicaid have been provided with continuous coverage. He and others haven’t been required to demonstrate they are still eligible for the coverage. Now that those rules are ending.
Starting April 1, people need to complete a redetermination showing that they qualify for the coverage.
Article continues after...
Yesterday's Most Read Articles
 Football helmet maker buys Lebanon’s Simbex
Football helmet maker buys Lebanon’s Simbex
 James Parker granted parole for his role in Dartmouth professors’ stabbing deaths
James Parker granted parole for his role in Dartmouth professors’ stabbing deaths
 Zantop daughter: ‘I wish James' family the best and hope that they are able to heal’
Zantop daughter: ‘I wish James' family the best and hope that they are able to heal’
 Kenyon: Dartmouth alumni join union-busting effort
Kenyon: Dartmouth alumni join union-busting effort
 Parker up for parole more than 2 decades after Dartmouth professor stabbing deaths
Parker up for parole more than 2 decades after Dartmouth professor stabbing deaths
 Through new school partnerships, CRREL seeks to educate young scientists
Through new school partnerships, CRREL seeks to educate young scientists
The change, required under federal rules, leaves more than 72,000 Granite Staters vulnerable to losing their coverage because they have not yet completed paperwork to inform the state of whether or not they still qualify for the program. Tens of thousands of Vermonters may also be at risk of losing coverage. As part of the renewal process that will happen gradually over the coming months, people covered by Medicaid will need to demonstrate that they income-qualify for the program.
Single adults must have an income of less than $18,075 annually, or $36,908 for a four-person household, to qualify for Medicaid, or 138% of the federal poverty level, according to benefits.gov. Pregnant people and children also can qualify for Medicaid at higher income limits.
Health officials in both states say they are working to notify Medicaid beneficiaries ahead of the change and they seek to ensure that those who qualify for coverage continue to get it and to help those that don’t to find coverage elsewhere.
Henry Lipman, Medicaid director at the New Hampshire Department of Health and Human Services, told reporters in a Zoom call on Tuesday that his department was using the data it has to delay the required recertification for those who are most vulnerable and ill.
“Those people who are most at risk for their health occur a bit later in the process,” he said.
Lipman said that those who are poised to lose their Medicaid coverage will have access to the federal health care exchange during a special enrollment period before their coverage ends. Comparing the difference in the state’s Medicaid enrollment from pre-pandemic numbers to current numbers, Lipman estimates that 64,000 people may no longer qualify for Medicaid by the end of the year.
“A lot of these people we hope will be Marketplace candidates,” he said, referring to the online health care exchange, healthcare.gov.
Ginger Irish, a spokeswoman for the Department of Vermont Health Access, said that the department cannot predict how many Vermonters will no longer be eligible for Medicaid after the “unwind.” But since January 2020, an additional 36,654 Vermonters have been covered by Medicaid.
Those who no longer qualify may still qualify for subsidies on the online Marketplace, Vermont Health Connect, vermonthealthconnect.gov, which may bring down the monthly premiums to zero or close to it, she said in an email.
“We have been diligently preparing our staff and systems for April, when we may begin to ‘unwind’ from continuous Medicaid coverage for Vermonters,” Andrea De La Bruere, commissioner of the Department of Vermont Health Access, said in an emailed statement. “This requires consistent, effective outreach to Vermonters to help them understand how their health coverage may be changing and make every effort to offer them opportunities to remain insured.”
New Hampshire has notified those who are at risk of losing their coverage by letter and ramped up its call center to help people navigate this change. Vermont also has sent Medicaid participants letters.
“Our mission here is if you should have coverage, we don’t want you to lose it,” Lipman said.
If people are uninsured, it can mean that hospitals and other providers have to provide care without reimbursement from providers or patients themselves. That uncompensated care can hit health care providers’ bottom lines, and if people avoid getting care due to the cost, that can affect their health, Lipman said.
“We really need workforce in this state and keeping our workforce healthy is an important thing,” he said.
For his part, Shumway, who is working with a group called the Nonviolent Medicaid Army, a multi-state initiative that is coordinated in Vermont by the Vermont Workers’ Center, hopes that this Medicaid change will inspire a broader conversation about how health care costs are covered.
“I along with folks across the state are getting together to talk to (ask) the question about universal health care,” he said. “... Why don’t we have it?”
The Department of Vermont Health Access is scheduled to host a virtual town hall, “What is the Medicaid unwind?” on Friday from noon-1 p.m. The session will be online at https://bit.ly/VTunwind.
Nora Doyle-Burr can be reached at ndoyleburr@vnews.com or 603-727-3213.

 Some families find freedom with Newport microschool
Some families find freedom with Newport microschool Woodstock Aqueduct Company seeks to double water rates
Woodstock Aqueduct Company seeks to double water rates
