Primary care doctors harder to find, as many in the Upper Valley are not taking new patients
| Published: 08-11-2022 10:58 PM |
LEBANON — In an ideal world, everyone would have a primary care provider they know and trust and see regularly.
But an ongoing workforce shortage in primary care means that many people in the Upper Valley are struggling to find that trusted provider, leaving some scrambling to get medication refilled, or find assistance managing their diabetes or monitoring their blood pressure.
Nathalie Hebert, one of two nurse practitioners at the Good Neighbor Health Clinic in White River Junction, said the practice, which serves people without insurance or who are underinsured, has increasingly been fielding calls from people who have health insurance but who are unable to find a primary care provider in a timely manner.
Over the past five or six months, Hebert, who also serves as operations manager for the medical clinic, said she’s seen the length of the time to establish care grow. When Dartmouth Hitchcock clinics in the Upper Valley placed a pause on accepting new primary care patients this spring, Hebert said Good Neighbor’s call volume increased about 15%. About half of those patients can be referred elsewhere, but she said the other half need to be seen there. Among the most pressing needs are medication refills, including psychiatric medications, she said.
“Some people do have needs that are rather pressing,” Hebert said.
For example, Hebert said she recently received a call from a social worker trying to help a man who was recently released from prison find care. The man was able to get an appointment to establish care at Mt. Ascutney Hospital and Health Center, which has practices in Windsor and Woodstock, but it was six months out. Hebert said Good Neighbor agreed to help the man with some refills of psychiatric medications on a temporary basis until he was able to establish a permanent primary care home.
“That’s very typical of what we are seeing at the moment,” Hebert said.
Taking on such a patient adds to the burden placed on the clinic’s volunteers.
Article continues after...
Yesterday's Most Read Articles
“It’s really a difficult time at the moment for people providing primary care,” Hebert said. “There are not enough of them (and they’re) seeing more patients then they kindly come and volunteer.”
She said the clinic is having a hard time recruiting new volunteers because primary care providers are “feeling really stretched thin.”
A primary care doctor, nurse practitioner or physician assistant “is supposed to look at us in the most holistic way that western medicine does,” Alice Ely, the executive director of the Public Health Council of the Upper Valley, said.
“Primary care is really important because it’s the place where people feel like somebody understands their whole health picture and for many, many people, particularly lower income, it’s really the major place they get care,” Ely said. “They may not choose to see specialists because they’re afraid they can’t afford them. Primary care is the place where most chronic disease management occurs. It’s important.”
Without primary care, people who are generally well for the most part will figure out how to stay well, Ely said. But people with chronic conditions may get sicker while they wait.
As people get sicker, they may be unable to do things they once were such as take care of their families or work.
That “becomes a burden on all of us,” she said.
This spring, citing an increase in demand from new residents, a workforce shortage and backlogs related to delayed care amid the COVID-19 pandemic, Dartmouth Health, the Upper Valley’s largest provider of health care services, placed a pause on scheduling new appointments for patients at clinics at Dartmouth Hitchcock Medical Center and on Heater Road and in Lyme; and DH-staffed clinics in southwestern Vermont — including those in Bennington, Manchester Center and Wilmington.
In recent weeks, however, it has opened up “limited access, at a slower pace, in an effort to onboard the new providers, reassign patients who are already established in the practices and work through our new patient wait list,” Audra Burns, a DH spokeswoman, said. “We encourage patients who are looking to establish with a new primary care to please call and they will be contacted as soon as an appointment is available.”
The increased access is possible due to the Lebanon primary care sites welcoming several new providers since July, others are expected to start in the next several months, Burns said. As of Tuesday, DH still had nearly 100 openings for positions in primary care in Lebanon, according to its online job site.
Jeffrey O’Brien, the chief operating officer of DHMC, said in a webinar hosted by U.S. News & World Report late last month that DHMC, which employs 9,000 people, has struggled with staffing, partly because of its rural location, as well as a “talent gap” that he attributed to people falling out of the workforce amid the pandemic and a dearth of people coming in to replace them. Issues such as housing and child care have further compounded the problem.
The workforce shortage has administrative and non-clinical staff filling in behind the scenes. For example, O’Brien said, there “was a practice manager (in an) outpatient clinic working the dish line in the clinic. It’s that real.”
Meanwhile, New London Hospital, a member of the DH system, is only accepting new pediatric patients for primary care. But the Newport Health Center, which is owned by New London Hospital, is accepting both adult and pediatric primary care patients. Both locations had stopped accepting new primary care patients in February.
“We can’t say exactly how long the pause will be at the New London location, as we are currently in the recruitment process,” Timothy J. Lund, a New London Hospital spokesman, said. “Pinpointing the exact cause of the shortage in primary care providers is difficult to narrow down, especially considering this reaches far beyond a regional issue.”
Dr. Marcus Hampers, CEO of ClearChoiceMD Urgent Care, said the shortage in primary care providers is not new, but it has gotten worse.
Hampers attributed the shortage in providers to the cost of training not matching the income primary care providers earn in practice. He said the shortage tends to be worse in poorer, more rural communities.
The “primary care physicians who are retiring, they’re not being replaced,” he said. “We’re not seeing these young professionals choosing primary care.”
Like the providers at Good Neighbor, ClearChoice, which has more than 15 locations across northern New England, sees patients who are unable to get in to see a primary care provider, but who are looking to have medication refilled, or to have their glucose level or blood pressure checked.
Hampers said he is considering setting up a program to “tee up a patient for a visit with their new primary care provider.”
Such a visit would include a routine physical exam, as well as routine lab work. Such work might help a primary care provider sort out which patients need to be seen sooner than others, he said.
“We think that we can work in sync with the local primary care practices,” he said.
One outlier among primary care options in the Upper Valley is Family Health Center in Lebanon. The small, privately owned practice sits off Mechanic Street. It has a total of less than a dozen employees, including two physicians and two physician assistants. They see as many as 900 patients a month but would like to hire another physician and see more.
“We seem to be one of the only places that is accepting new patients,” Kathy Bean, Family Health’s practice manager, said. “It’s quite a situation that primary care is in right now. It’s terrible.”
Since the practice put out a notice on its Facebook page in May that it was accepting new patients, it regularly gets calls from people seeking a primary care provider. Bean said she sometimes gets calls from Dartmouth Health employees who can’t find primary care providers for themselves.
While Family Health can usually get in new patients within a couple of weeks, they are not able to accept people on pain medication or with severe mental illness. They also ask people to call their insurance company in advance to see if they are within network.
“Some of them come and pay out of pocket because they need primary care,” Bean said of patients with private insurance that doesn’t include Family Health in their networks.
The practice is up against several challenges, Bean said. Primary care is not reimbursed as well as specialty care. Public insurers, Medicare and Medicaid, reimburse providers at especially low rates. The practice is still trying to recover from the early days of the pandemic when fewer people were coming in for care. Some switched to telehealth visits, but those weren’t reimbursed by insurance companies as well as in-person visits.
“You’re in a Catch-22 situation,” Bean said. “Whatever you do doesn’t help your bottom line.”
Employees have been out with COVID-19 at various times over the past couple of years and they sometimes go on vacation, “which is wonderful,” Bean said. “But we don’t see patients when people are on vacation.”
For now, the new patients are helping the practice, which first opened in 1972, to keep the doors open, Bean said. But it’s “hard to predict what the future’s going to be.”
Nora Doyle-Burr can be reached at ndoyleburr@vnews.com or 603-727-3213.

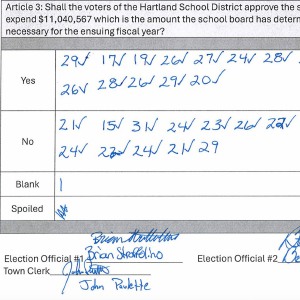 Hartland voters successfully petition for school budget revote
Hartland voters successfully petition for school budget revote 
