Latest News
 Editorial: Chris Sununu’s moral vacuum
Editorial: Chris Sununu’s moral vacuum
 Local Roundup: Rivendell extends baseball win streak
Local Roundup: Rivendell extends baseball win streak
 2024 Upper Valley high school softball guide
2024 Upper Valley high school softball guide

Out & About: Vermont Center for Ecostudies continues Backyard Tick Project
WHITE RIVER JUNCTION — The Vermont Center for Ecostudies is looking for people who are willing to allow researchers to study their lawns as part of the Upper Valley Backyard Tick Project.Jason Hill, a quantitative ecologist at the White River...

Some families find freedom with Newport microschool
NEWPORT — Tucked in the basement of Newport’s Epiphany Episcopal Church, Micah Studios is a newcomer to the Upper Valley’s alternative education landscape.Founded in the fall of 2023 by two educators disillusioned with the town’s public school system,...
Sports

2024 Upper Valley high school girls lacrosse guide
Two words best describe Upper Valley high school girls lacrosse: quality and consistency.All four squads made the playoffs last spring. While none came home with a state title, Hanover and Woodstock made their finals, with the Wasps’ trip coming at...
 Football helmet maker buys Lebanon’s Simbex
Football helmet maker buys Lebanon’s Simbex
 2024 Upper Valley high school track and field guide
2024 Upper Valley high school track and field guide
 2024 HS boys lacrosse guide
2024 HS boys lacrosse guide
 Kenyon: Dartmouth alumni join union-busting effort
Kenyon: Dartmouth alumni join union-busting effort
Opinion

A Yankee Notebook: An inevitable and terminal move
Living three and a half hours apart, as we do, my dear friend Bea and I get to see each other about every two weeks or so, on average. This is almost without doubt an ideal arrangement, as our lifestyles are quite different, and neither of us could...
 Editorial: Gambling tarnishes America’s sporting life
Editorial: Gambling tarnishes America’s sporting life
 By the Way: A white nationalist’s many mistruths
By the Way: A white nationalist’s many mistruths
 Column: The age-old question of what to read
Column: The age-old question of what to read
 Editorial: Transparency wins in NH Supreme Court ruling
Editorial: Transparency wins in NH Supreme Court ruling

Photos

Preserving habitat in Etna
 Pitching in
Pitching in
 Picture day prep
Picture day prep
 Helping a good cause in Etna
Helping a good cause in Etna
 Spring cleaning
Spring cleaning
Arts & Life

Art Notes: After losing primary venues, JAG Productions persists
For much of its history, JAG Productions, the small, White River Junction theater company that specializes in telling stories from deep inside the black, queer, American experience, has had to be nimble. Company founder Jarvis Antonio Green has...
 Over Easy: Marvels in the heavens, and in the yard
Over Easy: Marvels in the heavens, and in the yard
 Art Notes: The Pilgrims to perform ‘last’ show Saturday in Hanover
Art Notes: The Pilgrims to perform ‘last’ show Saturday in Hanover
 Upper Valley residents witness total eclipse
Upper Valley residents witness total eclipse
Obituaries
 Terrance W. Hood Sr.
Terrance W. Hood Sr.
Enfield, NH - Terrance W. Hood Sr., 63, passed away unexpectedly Saturday April 6, 2024 at Dartmouth Health. He was born in Barre City, VT and was raised by Arthur & Marjorie (Salomaa) Hood... remainder of obit for Terrance W. Hood Sr.
 Veronica Alonzo
Veronica Alonzo
Lebanon, NH - Veronica Ann Alonzo died peacefully at Dartmouth Hitchcock Medical Center on April 10, 2024, in Lebanon NH at the age of 63. Veronica was born on May 6, 1960, in Orange, Calif... remainder of obit for Veronica Alonzo
 Elizabeth Allebach
Elizabeth Allebach
Hanover, NH - Elizabeth "Betty" Belle Peach Allebach, 91, beloved family member and friend to many, died peacefully at Kendal of Hanover on April 7, 2024. She was surrounded by many relativ... remainder of obit for Elizabeth Allebach
 Marion D. Barr
Marion D. Barr
Weathersfield, VT - Marion D. Barr, age 88, passed Sunday, March 10, 2024. A service will be held at 10am on Saturday, April 27, 2024, at the Brownsville Community Church. Knight Funera... remainder of obit for Marion D. Barr

 Woodstock Aqueduct Company seeks to double water rates
Woodstock Aqueduct Company seeks to double water rates
 Apply to join the Valley News Reader Advisory Board
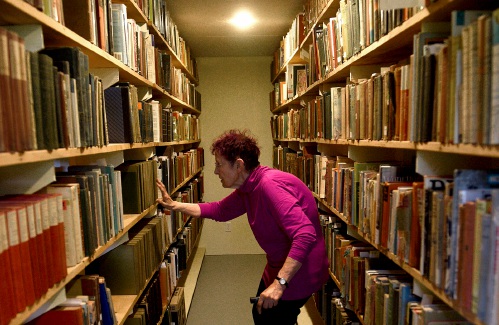
Apply to join the Valley News Reader Advisory Board A Life: Priscilla Sears ‘was bold enough to be very demanding’
A Life: Priscilla Sears ‘was bold enough to be very demanding’ Kenyon: Dismas House celebrates 10 years of fresh starts in Hartford
Kenyon: Dismas House celebrates 10 years of fresh starts in Hartford Editorial: Accounting can now begin in Claremont police case
Editorial: Accounting can now begin in Claremont police case
 Amid financial difficulties, Lebanon-based Revels North cancels midwinter show
Amid financial difficulties, Lebanon-based Revels North cancels midwinter show 
