
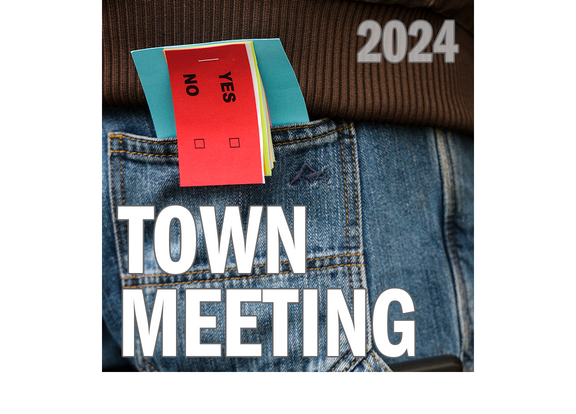
Hartford voters approve school budget and building repair bond
HARTFORD — Voters approved the school district’s $51 million budget, as well as a $21 million bond for facilities repairs in Australian ballot voting Monday.The budget passed 728-622, or about 54% to 46%.The bond passed more narrowly, 712-634, or...

Kenyon: Dartmouth alumni join union-busting effort
Dartmouth President Sian Leah Beilock has made it clear the college views its men’s basketball players — and their recent historic vote to unionize — as a threat to ….Fill in the blank.The college’s bottom line? The status quo? The misconception that...
Most Read
 Starbucks store planned for Route 120 at Centerra
Starbucks store planned for Route 120 at Centerra
 Canaan Elementary School has new principal
Canaan Elementary School has new principal
 City plans to widen and replace bridge on Trues Brook Road
City plans to widen and replace bridge on Trues Brook Road
 Enterprise: Upper Valley pet sitters discuss business growth, needs
Enterprise: Upper Valley pet sitters discuss business growth, needs
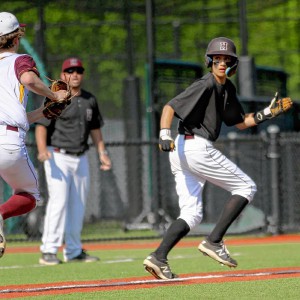 2024 Upper Valley high school baseball guide
2024 Upper Valley high school baseball guide
Editors Picks
 Town Meeting 2024: Previews and results of Upper Valley meetings and votes
Town Meeting 2024: Previews and results of Upper Valley meetings and votes
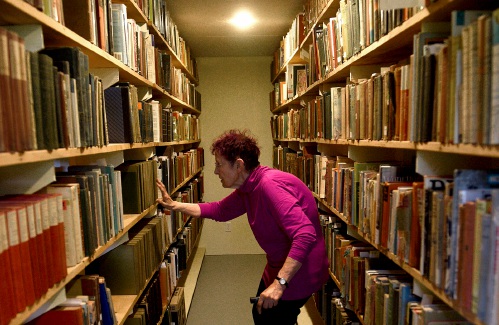
 A Life: Priscilla Sears ‘was bold enough to be very demanding’
A Life: Priscilla Sears ‘was bold enough to be very demanding’
 Kenyon: Dismas House celebrates 10 years of fresh starts in Hartford
Kenyon: Dismas House celebrates 10 years of fresh starts in Hartford
 Editorial: Accounting can now begin in Claremont police case
Editorial: Accounting can now begin in Claremont police case
Sports

2024 HS boys lacrosse guide
Once you’ve finally been to the top of the mountain, what do you do for an encore?That’s the challenge facing the Hartford High boys lacrosse program this spring. After multiple attempts that came up short, the Hurricanes ran the table en route to...
 2024 Upper Valley high school baseball guide
2024 Upper Valley high school baseball guide
 Ex-Virginia assistant Kirwan latest to step into the Big Green breach
Ex-Virginia assistant Kirwan latest to step into the Big Green breach
 Durham combines strength, fitness on the trails
Durham combines strength, fitness on the trails
 Out & About: Thin ice puts future of Upper Valley skating trails in jeopardy
Out & About: Thin ice puts future of Upper Valley skating trails in jeopardy
Opinion

A Yankee Notebook: An inevitable and terminal move
Living three and a half hours apart, as we do, my dear friend Bea and I get to see each other about every two weeks or so, on average. This is almost without doubt an ideal arrangement, as our lifestyles are quite different, and neither of us could...
 Editorial: Gambling tarnishes America’s sporting life
Editorial: Gambling tarnishes America’s sporting life
 By the Way: A white nationalist’s many mistruths
By the Way: A white nationalist’s many mistruths
 Column: The age-old question of what to read
Column: The age-old question of what to read
 Editorial: Transparency wins in NH Supreme Court ruling
Editorial: Transparency wins in NH Supreme Court ruling

Photos

Acoustic music jam in White River Junction
 Stocking Windsor’s Kennedy Pond
Stocking Windsor’s Kennedy Pond
 Quechee Gorge Bridge construction begins
Quechee Gorge Bridge construction begins
 Getting a lift in South Royalton
Getting a lift in South Royalton
 Lebanon’s reconstruction project
Lebanon’s reconstruction project
Arts & Life

Over Easy: Marvels in the heavens, and in the yard
It was Traffic vs. the Eclipse on Monday, a showdown of celestial proportions. Would I risk everything like Marco Polo who bravely set out to see the world, or follow the example of his brother Rocco, who said their hometown of Venice was “plenty good...
 Art Notes: The Pilgrims to perform ‘last’ show Saturday in Hanover
Art Notes: The Pilgrims to perform ‘last’ show Saturday in Hanover
 Upper Valley residents witness total eclipse
Upper Valley residents witness total eclipse
 Sunshine, snacks and laughs features of Bugbee’s solar eclipse party
Sunshine, snacks and laughs features of Bugbee’s solar eclipse party
Obituaries
 Joseph M. DeChant
Joseph M. DeChant
New London, NH - Joseph M. DeChant, age 89, passed Tuesday, February 13, 2024. A memorial service for Joseph M. DeChant, 89, who died on February 13, 2024, will be held on Saturday, May... remainder of obit for Joseph M. DeChant
 Barbara Champagne
Barbara Champagne
reading, VT - A graveside service for Barbara "Bobbi" Champagne who passed away on January 26, 2024 will be held in St Mary Cemetery in Claremont, NH on Saturday, April 20th at 1PM. ... remainder of obit for Barbara Champagne
 Josephine Tansey
Josephine Tansey
Josephine (Bertino) Tansey Rutland, VT - Josephine (Bertino) Tansey died Saturday morning (April 13, 2024) at the Mountain View Center Genesis Healthcare in Rutland, VT. Mrs. Tansey was born... remainder of obit for Josephine Tansey
 Sharon Nordgren
Sharon Nordgren
Hanover, NH - Sharon L. Nordgren 10/21/1943-02/10/2024 Sharon L. Nordgren passed away on February 10th, 2024 in Hanover, New Hampshire. She was 80 years old. Sharon was born Octobe... remainder of obit for Sharon Nordgren

 Art Notes: After losing primary venues, JAG Productions persists
Art Notes: After losing primary venues, JAG Productions persists
 2024 Upper Valley high school track and field guide
2024 Upper Valley high school track and field guide
 With less than three months left, NH casino hasn’t found a buyer
With less than three months left, NH casino hasn’t found a buyer
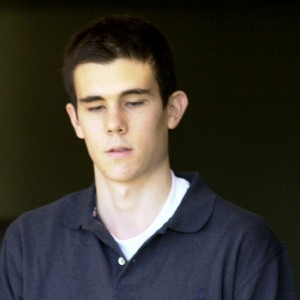 Parker up for parole more than 2 decades after Dartmouth professor stabbing deaths
Parker up for parole more than 2 decades after Dartmouth professor stabbing deaths
 A former NH youth detention center resident testifies about ‘hit squad’ attack
A former NH youth detention center resident testifies about ‘hit squad’ attack
 Windsor baseball’s annual gauntlet begins with Hartford defeat
Windsor baseball’s annual gauntlet begins with Hartford defeat

 Amid financial difficulties, Lebanon-based Revels North cancels midwinter show
Amid financial difficulties, Lebanon-based Revels North cancels midwinter show 
