
Crowd turns out to honor late Ascutney Fire Chief Darrin Spaulding
WEATHERSFIELD — An estimated 1,500 people filled the Weathersfield School gym for a funeral for Ascutney Fire Chief Darrin Spaulding on Saturday.Among those attending were Spaulding’s family members, firefighters in uniform, and others wishing to pay...

Pick a sport and Pete DePalo’s has probably officiated it over the past 40-plus years
Pete DePalo spent his first 15 years living on Coney Island in the New York City borough of Brooklyn, home of America’s first large-scale amusement park. His family moved to the Upper Valley and his life since has been filled with games.Soccer games....
Most Read
 Zantop daughter: ‘I wish James' family the best and hope that they are able to heal’
Zantop daughter: ‘I wish James' family the best and hope that they are able to heal’
 Crowd turns out to honor late Ascutney Fire Chief Darrin Spaulding
Crowd turns out to honor late Ascutney Fire Chief Darrin Spaulding
 A Life: For Kevin Jones ‘everything was geared toward helping other people succeed’
A Life: For Kevin Jones ‘everything was geared toward helping other people succeed’
 Pick a sport and Pete DePalo’s has probably officiated it over the past 40-plus years
Pick a sport and Pete DePalo’s has probably officiated it over the past 40-plus years
 Out & About: Vermont Center for Ecostudies continues Backyard Tick Project
Out & About: Vermont Center for Ecostudies continues Backyard Tick Project
Editors Picks
 Some families find freedom with Newport microschool
Some families find freedom with Newport microschool
 A Life: For Kevin Jones ‘everything was geared toward helping other people succeed’
A Life: For Kevin Jones ‘everything was geared toward helping other people succeed’
 Editorial: Chris Sununu’s moral vacuum
Editorial: Chris Sununu’s moral vacuum
Sports

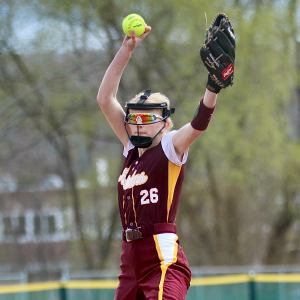
2024 Upper Valley high school softball guide
When it comes to Upper Valley high school softball, one program stirs the proverbial championship drink.In three years under coach Chuck Simmons, Oxbow High has reeled off 49 wins in 53 games and raced relatively unimpeded to state honors each time....
 2024 Upper Valley high school girls lacrosse guide
2024 Upper Valley high school girls lacrosse guide
 Football helmet maker buys Lebanon’s Simbex
Football helmet maker buys Lebanon’s Simbex
 2024 Upper Valley high school track and field guide
2024 Upper Valley high school track and field guide
 2024 HS boys lacrosse guide
2024 HS boys lacrosse guide
Opinion

A Yankee Notebook: An inevitable and terminal move
Living three and a half hours apart, as we do, my dear friend Bea and I get to see each other about every two weeks or so, on average. This is almost without doubt an ideal arrangement, as our lifestyles are quite different, and neither of us could...
 Editorial: Gambling tarnishes America’s sporting life
Editorial: Gambling tarnishes America’s sporting life
 By the Way: A white nationalist’s many mistruths
By the Way: A white nationalist’s many mistruths
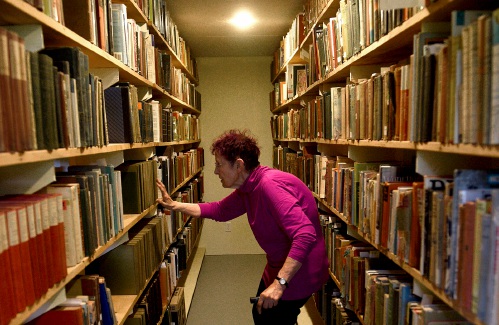 Column: The age-old question of what to read
Column: The age-old question of what to read
 Editorial: Transparency wins in NH Supreme Court ruling
Editorial: Transparency wins in NH Supreme Court ruling

Photos

Preserving habitat in Etna
 Pitching in
Pitching in
 Picture day prep
Picture day prep
 Helping a good cause in Etna
Helping a good cause in Etna
 Spring cleaning
Spring cleaning
Arts & Life

How a hurricane and a cardinal launched a UVM professor on a new career path
Before Hurricane Katrina hit her newly adopted city of New Orleans in 2005, Trish O’Kane knew next to nothing about the environment — let alone birds.O’Kane had spent much of her life working as an investigative human rights journalist in Central...
 Out & About: Vermont Center for Ecostudies continues Backyard Tick Project
Out & About: Vermont Center for Ecostudies continues Backyard Tick Project
 Art Notes: After losing primary venues, JAG Productions persists
Art Notes: After losing primary venues, JAG Productions persists
 Over Easy: Marvels in the heavens, and in the yard
Over Easy: Marvels in the heavens, and in the yard
Obituaries
 Russell Haviland
Russell Haviland
West Newbury, VT - Russ Haviland passed away peacefully in North Haverhill, New Hampshire on April 18, 2024. He was born on March 17, 1941, in Brattleboro, Vermont to E. Randall Haviland and Gretchen (Shaw) Haviland. Russ's time was a l... remainder of obit for Russell Haviland
 Constance Barth
Constance Barth
Brownsville, VT - Constance Rae Zullo Barth passed away April 21, 2024. She was 81. The world is significantly less without her and infinitely more for the gifts her life brought us. Born August 31, 1942 in Claremont, New Hampshire, ... remainder of obit for Constance Barth
 Adrian W. Frary Jr.
Adrian W. Frary Jr.
Adrian W. Frary, Jr. Tunbridge, VT - Adrian W. Frary, Jr., age 98, passed Wednesday, April 3, 2024. A graveside memorial service for Adrian will be held Sunday, April 28, 2024 at 2pm with refreshments and fellowship to follow at the Roy... remainder of obit for Adrian W. Frary Jr.
 Elaine J. George
Elaine J. George
White River Jct., VT - Elaine Jane (Viens) George passed away April 21, 2024, surrounded by her loving family and friends. Elaine was born on Dec. 12, 1934, in Springfield, Mass., the ninth child of George and Delima (Ashline) Viens, Sr... remainder of obit for Elaine J. George


 Former principal of South Royalton School released from prison
Former principal of South Royalton School released from prison
 Upper Valley residents among advocates for NH aid-in-dying bill
Upper Valley residents among advocates for NH aid-in-dying bill
 NH man convicted of killing daughter, 5, ordered to be at sentencing after skipping trial
NH man convicted of killing daughter, 5, ordered to be at sentencing after skipping trial
 Lebanon girls lacrosse prevails over Coe-Brown
Lebanon girls lacrosse prevails over Coe-Brown
 Local roundup: Lebanon softball sweeps wins from Souhegan, Stark
Local roundup: Lebanon softball sweeps wins from Souhegan, Stark
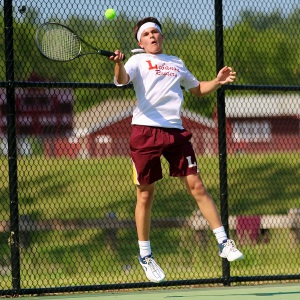 2024 Upper Valley high school tennis guide
2024 Upper Valley high school tennis guide

 Amid financial difficulties, Lebanon-based Revels North cancels midwinter show
Amid financial difficulties, Lebanon-based Revels North cancels midwinter show 
