Latest News
 Football helmet maker buys Lebanon’s Simbex
Football helmet maker buys Lebanon’s Simbex
 2024 Upper Valley high school track and field guide
2024 Upper Valley high school track and field guide

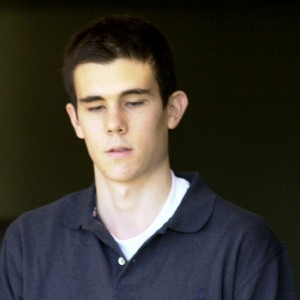
James Parker granted parole for his role in Dartmouth professors’ stabbing deaths
CONCORD — A man who has served more than half of his life in prison for his role in the 2001 stabbing deaths of two married Dartmouth College professors as part of a plan to rob and kill people before fleeing overseas was granted parole Thursday.James...

Through new school partnerships, CRREL seeks to educate young scientists
LYME — On a raw, not-quite-spring New England afternoon, four seventh and eighth graders in the New Hampshire Academy of Science’s (NHAS) after-school program clustered around a computer, choosing images of orchids for a poster they’re designing to...
Most Read
 Kenyon: Dartmouth alumni join union-busting effort
Kenyon: Dartmouth alumni join union-busting effort
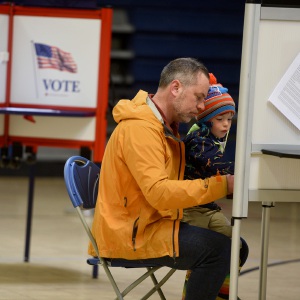 Hartford voters approve school budget and building repair bond
Hartford voters approve school budget and building repair bond
 Starbucks store planned for Route 120 at Centerra
Starbucks store planned for Route 120 at Centerra
 Local Roundup: Hanover pitcher throws a perfect game
Local Roundup: Hanover pitcher throws a perfect game
 Parker up for parole more than 2 decades after Dartmouth professor stabbing deaths
Parker up for parole more than 2 decades after Dartmouth professor stabbing deaths
Editors Picks
 Town Meeting 2024: Previews and results of Upper Valley meetings and votes
Town Meeting 2024: Previews and results of Upper Valley meetings and votes
 A Life: Priscilla Sears ‘was bold enough to be very demanding’
A Life: Priscilla Sears ‘was bold enough to be very demanding’
 Kenyon: Dismas House celebrates 10 years of fresh starts in Hartford
Kenyon: Dismas House celebrates 10 years of fresh starts in Hartford
 Editorial: Accounting can now begin in Claremont police case
Editorial: Accounting can now begin in Claremont police case
Sports

2024 HS boys lacrosse guide
Once you’ve finally been to the top of the mountain, what do you do for an encore?That’s the challenge facing the Hartford High boys lacrosse program this spring. After multiple attempts that came up short, the Hurricanes ran the table en route to...
 Kenyon: Dartmouth alumni join union-busting effort
Kenyon: Dartmouth alumni join union-busting effort
 Windsor baseball’s annual gauntlet begins with Hartford defeat
Windsor baseball’s annual gauntlet begins with Hartford defeat
 2024 Upper Valley high school baseball guide
2024 Upper Valley high school baseball guide
 Ex-Virginia assistant Kirwan latest to step into the Big Green breach
Ex-Virginia assistant Kirwan latest to step into the Big Green breach
Opinion

A Yankee Notebook: An inevitable and terminal move
Living three and a half hours apart, as we do, my dear friend Bea and I get to see each other about every two weeks or so, on average. This is almost without doubt an ideal arrangement, as our lifestyles are quite different, and neither of us could...
 Editorial: Gambling tarnishes America’s sporting life
Editorial: Gambling tarnishes America’s sporting life
 By the Way: A white nationalist’s many mistruths
By the Way: A white nationalist’s many mistruths
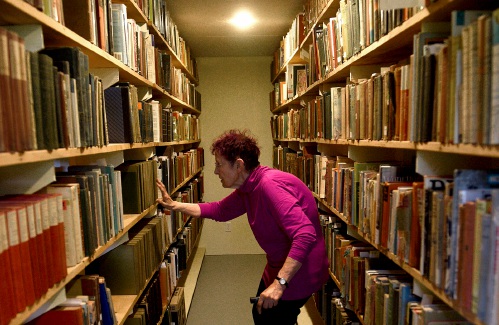 Column: The age-old question of what to read
Column: The age-old question of what to read
 Editorial: Transparency wins in NH Supreme Court ruling
Editorial: Transparency wins in NH Supreme Court ruling

Photos

Acoustic music jam in White River Junction
 Stocking Windsor’s Kennedy Pond
Stocking Windsor’s Kennedy Pond
 Quechee Gorge Bridge construction begins
Quechee Gorge Bridge construction begins
 Getting a lift in South Royalton
Getting a lift in South Royalton
 Lebanon’s reconstruction project
Lebanon’s reconstruction project
Arts & Life

Over Easy: Marvels in the heavens, and in the yard
It was Traffic vs. the Eclipse on Monday, a showdown of celestial proportions. Would I risk everything like Marco Polo who bravely set out to see the world, or follow the example of his brother Rocco, who said their hometown of Venice was “plenty good...
 Art Notes: The Pilgrims to perform ‘last’ show Saturday in Hanover
Art Notes: The Pilgrims to perform ‘last’ show Saturday in Hanover
 Upper Valley residents witness total eclipse
Upper Valley residents witness total eclipse
 Sunshine, snacks and laughs features of Bugbee’s solar eclipse party
Sunshine, snacks and laughs features of Bugbee’s solar eclipse party
Obituaries
 Lisa Gurney
Lisa Gurney
Newbury, VT - Lisa Marie Gurney, age 55, passed Thursday, March 7, 2024. There will be a graveside service on Thursday, May 2, 2024, at the New Oxbow Cemetery in Newbury, VT, at 10 AM. ... remainder of obit for Lisa Gurney
 Megan Mattern
Megan Mattern
Midland, TX - Megan Mattern, 44, passed away on March 15, 2024, at Dartmouth Hitchcock Medical Center, after a valiant fight with cancer. Born December 6, 1979 to Wes and Susan Mattern, Meg... remainder of obit for Megan Mattern
 James R. Thibodeau
James R. Thibodeau
Leland, NC - James R. Thibodeau, age 75, passed Saturday, April 13, 2024. A full obituary will be published in an upcoming edition of the Valley News. Ricker Funeral Home has assist... remainder of obit for James R. Thibodeau
 Beverly Vaughan
Beverly Vaughan
East Thetford, VT - Beverly Vaughan, 76, of East Thetford, VT, died unexpectedly on Sunday, April 14, 2024. She was born on December 18,1947, to Floyd and Bessie (Minor) Dexter. She gre... remainder of obit for Beverly Vaughan

 Art Notes: After losing primary venues, JAG Productions persists
Art Notes: After losing primary venues, JAG Productions persists
 With less than three months left, NH casino hasn’t found a buyer
With less than three months left, NH casino hasn’t found a buyer
 A former NH youth detention center resident testifies about ‘hit squad’ attack
A former NH youth detention center resident testifies about ‘hit squad’ attack

 Amid financial difficulties, Lebanon-based Revels North cancels midwinter show
Amid financial difficulties, Lebanon-based Revels North cancels midwinter show 
