
Upper Valley winter shelters kept dozens warm and dry
LEBANON — Organizers of two new emergency shelters, which kept dozens of Upper Valley residents off the streets this winter, are reflecting on the season and sorting out how to continue the service.Earlier this month, Lebanon’s emergency shelter for...

JAG Productions announces closure, citing ‘crisis facing the arts’
JAG Productions, the White River Junction theater company that has championed the work of Black, queer and trans artists, announced last week that it is closing in June after eight years of bringing groundbreaking work to the Upper Valley.Jarvis...
Most Read
 Crowd turns out to honor late Ascutney Fire Chief Darrin Spaulding
Crowd turns out to honor late Ascutney Fire Chief Darrin Spaulding
 Former principal of South Royalton School released from prison
Former principal of South Royalton School released from prison
 Pick a sport and Pete DePalo’s has probably officiated it over the past 40-plus years
Pick a sport and Pete DePalo’s has probably officiated it over the past 40-plus years
 Upper Valley residents among advocates for NH aid-in-dying bill
Upper Valley residents among advocates for NH aid-in-dying bill
 NH man convicted of killing daughter, 5, ordered to be at sentencing after skipping trial
NH man convicted of killing daughter, 5, ordered to be at sentencing after skipping trial
Editors Picks
 Some families find freedom with Newport microschool
Some families find freedom with Newport microschool
 A Life: For Kevin Jones ‘everything was geared toward helping other people succeed’
A Life: For Kevin Jones ‘everything was geared toward helping other people succeed’
 Kenyon: Hanover stalls on police records request
Kenyon: Hanover stalls on police records request
 Editorial: Chris Sununu’s moral vacuum
Editorial: Chris Sununu’s moral vacuum
Sports

Woodstock boys lax defense steps up, holds off Hartford
WHITE RIVER JUNCTION — Monday night’s boys lacrosse game between host Hartford High and Woodstock came down to the final minute, with the Wasps prevailing, 11-10.The Vermont inter-division clash might have been decided, however, by a pair of goals at...
 Pick a sport and Pete DePalo’s has probably officiated it over the past 40-plus years
Pick a sport and Pete DePalo’s has probably officiated it over the past 40-plus years
 Lebanon girls lacrosse prevails over Coe-Brown
Lebanon girls lacrosse prevails over Coe-Brown
 Local roundup: Lebanon softball sweeps wins from Souhegan, Stark
Local roundup: Lebanon softball sweeps wins from Souhegan, Stark
 2024 Upper Valley high school tennis guide
2024 Upper Valley high school tennis guide
Opinion

Editorial: Gambling tarnishes America’s sporting life
Hey, Major League Baseball, does the name Pete Rose ring a bell? Remember him, “Charlie Hustle”? One of the game’s greatest players, whom you banned for life in 1989 because he bet on baseball games?We ask because you have on your hands another...
 By the Way: A white nationalist’s many mistruths
By the Way: A white nationalist’s many mistruths
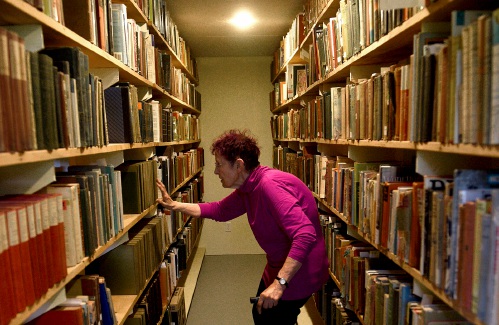 Column: The age-old question of what to read
Column: The age-old question of what to read
 Editorial: Transparency wins in NH Supreme Court ruling
Editorial: Transparency wins in NH Supreme Court ruling
 A Yankee Notebook: Among the crowds on vacation out West
A Yankee Notebook: Among the crowds on vacation out West

Photos

Ramping up their foraging
 Roadside assist in Bethel
Roadside assist in Bethel
 Preserving habitat in Etna
Preserving habitat in Etna
 Pitching in
Pitching in
 Picture day prep
Picture day prep
Arts & Life

How a hurricane and a cardinal launched a UVM professor on a new career path
Before Hurricane Katrina hit her newly adopted city of New Orleans in 2005, Trish O’Kane knew next to nothing about the environment — let alone birds.O’Kane had spent much of her life working as an investigative human rights journalist in Central...
 Out & About: Vermont Center for Ecostudies continues Backyard Tick Project
Out & About: Vermont Center for Ecostudies continues Backyard Tick Project
 Art Notes: After losing primary venues, JAG Productions persists
Art Notes: After losing primary venues, JAG Productions persists
 Over Easy: Marvels in the heavens, and in the yard
Over Easy: Marvels in the heavens, and in the yard
Obituaries
 Jane Elizabeth Rooney
Jane Elizabeth Rooney
Manchester, NH - Jane Elizabeth Rooney, who had a long career as a social worker and psychotherapist, died on March 28, 2024, at Mount Carmel Rehabilitation and Nursing Center in Manchester, NH. Jane was born in Framingham, Massachuset... remainder of obit for Jane Elizabeth Rooney
 Cory John MacElman
Cory John MacElman
Lebanon, NH - Cory John MacElman, age 39, passed Friday, April 19, 2024. Ricker Funeral Home of Lebanon, NH is assisting the family. ... remainder of obit for Cory John MacElman
 Michael F. Hoar
Michael F. Hoar
Enfield, NH - Michael F. Hoar, 75, passed away following a period of declining health on Sunday April 21st 2024. He was born to the late Francis & Rita (Frazer) Hoar and was raised in Stoneham, MA. Michael was an avid skier and had work... remainder of obit for Michael F. Hoar
 Russell Haviland
Russell Haviland
West Newbury, VT - Russ Haviland passed away peacefully in North Haverhill, New Hampshire on April 18, 2024. He was born on March 17, 1941, in Brattleboro, Vermont to E. Randall Haviland and Gretchen (Shaw) Haviland. Russ's time was a l... remainder of obit for Russell Haviland


 Hanover’s Perreard may soon capture the attention of collegiate coaches in two athletic pursuits
Hanover’s Perreard may soon capture the attention of collegiate coaches in two athletic pursuits
 Local Roundup: Hartford girls lacrosse gets decisive win over Colchester
Local Roundup: Hartford girls lacrosse gets decisive win over Colchester
 Republicans have made illegal immigration a top issue in NH — sometimes with misinformation
Republicans have made illegal immigration a top issue in NH — sometimes with misinformation
 Owner of Friesian horse facility ordered to pay care costs for seized animals
Owner of Friesian horse facility ordered to pay care costs for seized animals

 Amid financial difficulties, Lebanon-based Revels North cancels midwinter show
Amid financial difficulties, Lebanon-based Revels North cancels midwinter show 
