Latest News
 2024 Upper Valley high school girls lacrosse guide
2024 Upper Valley high school girls lacrosse guide

Zantop daughter: ‘I wish James' family the best and hope that they are able to heal’
HANOVER — One of Susanne and Half Zantop’s two daughters said Thursday that she tries to “compartmentalize” her personal grief over the loss of her parents from her attitude about the fate of James Parker, who was paroled on Thursday after serving the...

James Parker granted parole for his role in Dartmouth professors’ stabbing deaths
CONCORD — A man who has served more than half of his life in prison for his role in the 2001 stabbing deaths of two married Dartmouth College professors as part of a plan to rob and kill people before fleeing overseas was granted parole Thursday.James...
Most Read
 Football helmet maker buys Lebanon’s Simbex
Football helmet maker buys Lebanon’s Simbex
 James Parker granted parole for his role in Dartmouth professors’ stabbing deaths
James Parker granted parole for his role in Dartmouth professors’ stabbing deaths
 Zantop daughter: ‘I wish James' family the best and hope that they are able to heal’
Zantop daughter: ‘I wish James' family the best and hope that they are able to heal’
 Kenyon: Dartmouth alumni join union-busting effort
Kenyon: Dartmouth alumni join union-busting effort
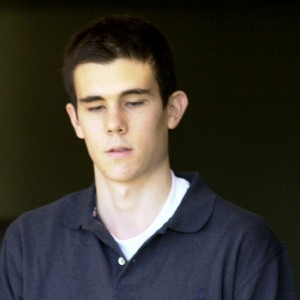 Parker up for parole more than 2 decades after Dartmouth professor stabbing deaths
Parker up for parole more than 2 decades after Dartmouth professor stabbing deaths
 Through new school partnerships, CRREL seeks to educate young scientists
Through new school partnerships, CRREL seeks to educate young scientists
Editors Picks
 Town Meeting 2024: Previews and results of Upper Valley meetings and votes
Town Meeting 2024: Previews and results of Upper Valley meetings and votes
 A Life: Priscilla Sears ‘was bold enough to be very demanding’
A Life: Priscilla Sears ‘was bold enough to be very demanding’
 Kenyon: Dismas House celebrates 10 years of fresh starts in Hartford
Kenyon: Dismas House celebrates 10 years of fresh starts in Hartford
 Editorial: Accounting can now begin in Claremont police case
Editorial: Accounting can now begin in Claremont police case
Sports

2024 Upper Valley high school track and field guide
As surely as snapping the finish-line tape signifies a winner, the Upper Valley is filled with high school track and field potential this spring.A number of area schools won outdoor titles last year, and some followed that up with indoor successes...
 Thetford tops Windsor in 19-18 softball slugfest
Thetford tops Windsor in 19-18 softball slugfest
 2024 HS boys lacrosse guide
2024 HS boys lacrosse guide
 Kenyon: Dartmouth alumni join union-busting effort
Kenyon: Dartmouth alumni join union-busting effort
 Windsor baseball’s annual gauntlet begins with Hartford defeat
Windsor baseball’s annual gauntlet begins with Hartford defeat
Opinion

A Yankee Notebook: An inevitable and terminal move
Living three and a half hours apart, as we do, my dear friend Bea and I get to see each other about every two weeks or so, on average. This is almost without doubt an ideal arrangement, as our lifestyles are quite different, and neither of us could...
 Editorial: Gambling tarnishes America’s sporting life
Editorial: Gambling tarnishes America’s sporting life
 By the Way: A white nationalist’s many mistruths
By the Way: A white nationalist’s many mistruths
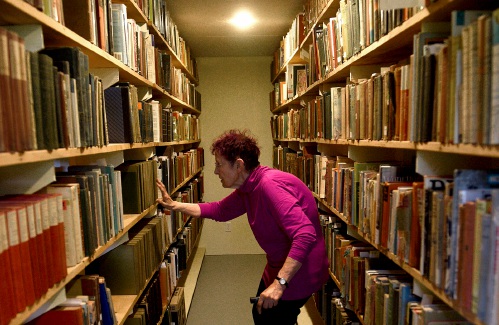 Column: The age-old question of what to read
Column: The age-old question of what to read
 Editorial: Transparency wins in NH Supreme Court ruling
Editorial: Transparency wins in NH Supreme Court ruling

Photos

Acoustic music jam in White River Junction
 Stocking Windsor’s Kennedy Pond
Stocking Windsor’s Kennedy Pond
 Quechee Gorge Bridge construction begins
Quechee Gorge Bridge construction begins
 Getting a lift in South Royalton
Getting a lift in South Royalton
 Lebanon’s reconstruction project
Lebanon’s reconstruction project
Arts & Life

Art Notes: After losing primary venues, JAG Productions persists
For much of its history, JAG Productions, the small, White River Junction theater company that specializes in telling stories from deep inside the black, queer, American experience, has had to be nimble. Company founder Jarvis Antonio Green has...
 Over Easy: Marvels in the heavens, and in the yard
Over Easy: Marvels in the heavens, and in the yard
 Art Notes: The Pilgrims to perform ‘last’ show Saturday in Hanover
Art Notes: The Pilgrims to perform ‘last’ show Saturday in Hanover
 Upper Valley residents witness total eclipse
Upper Valley residents witness total eclipse
Obituaries
 Douglas G. Whitcomb
Douglas G. Whitcomb
Hartland, VT - Douglas G. Whitcomb, age 84, passed Wednesday, February 21, 2024. Services will be held in The Vermont Veterans Memorial Cemetery Chapel in Randolph Center, VT, on Friday... remainder of obit for Douglas G. Whitcomb
 Edward Peter Rogenski
Edward Peter Rogenski
Newport, NH - Edward Peter Rogenski 11/10/1938 - 03/28/2024 Edward Peter Rogenski better known as Pete passed away peacefully at his home in Newport New Hampshire. He was 85 years old.... remainder of obit for Edward Peter Rogenski
 Harold Graham
Harold Graham
Woodsville, NH - Harold "Jack" John Graham, 95, passed away at his home on Monday, April 15, 2024, with family at his side. He was born in his family home on Savage Hill in Lisbon, NH on No... remainder of obit for Harold Graham
 Lisa Gurney
Lisa Gurney
Newbury, VT - Lisa Marie Gurney, age 55, passed Thursday, March 7, 2024. There will be a graveside service on Thursday, May 2, 2024, at the New Oxbow Cemetery in Newbury, VT, at 10 AM. ... remainder of obit for Lisa Gurney

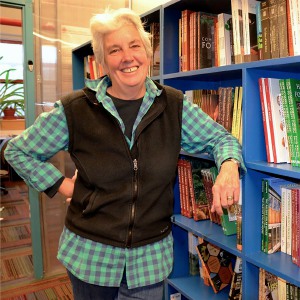 Chelsea Green to be sold to international publishing behemoth
Chelsea Green to be sold to international publishing behemoth

 Amid financial difficulties, Lebanon-based Revels North cancels midwinter show
Amid financial difficulties, Lebanon-based Revels North cancels midwinter show 
