Two Area Nursing Homes Were Sold: One Got Better, the Other Got Worse
| Published: 01-30-2017 10:59 AM |
White River Junction
Brookside Health and Rehabilitation, a 67-bed facility in White River Junction, has seen its overall rating by Medicare fall from five stars to two stars since August 2015, when it was purchased by a New York-based group of real estate investors and nursing home operators.
Five stars indicate a “much above average” rating, while two stars indicate “below average,” according to the U.S. Centers for Medicare and Medicaid Services, which awards the stars using data from state inspections and reports from nursing home operators.
“They appear to be on a downward path,” said Eric Avildsen, executive director of Vermont Legal Aid, which operates the state’s Long Term Care Ombudsman program. Problems showed up in Brookside’s last relicensing inspection, he said: “We’re taking it pretty seriously.”
Last year the ombudsman conducted five cases and received 14 complaints against Brookside, which Avildsen termed “a relatively high number.”
Hanover Terrace Health and Rehabilitation, a 100-bed facility in Hanover that was acquired by another New York-based owner about eight months ago, has endured its own troubles but is showing signs of progress, according to the home’s administrator and state and federal regulators.
Although Hanover Terrace has a one-star, or “much below average” rating, it performed well enough on recent inspections to qualify to exit from Medicare’s special-focus facility list of homes with “persistent poor quality of care,” according to Martha Chesley, who became Hanover Terrace’s administrator in July.
Hanover Terrace, which is currently the only New Hampshire nursing home on CMS’ special focus list, had no serious failings in its two most recent inspections, said Jake Leon, a spokesman for the New Hampshire Health and Human Services Department.
Article continues after...
Yesterday's Most Read Articles
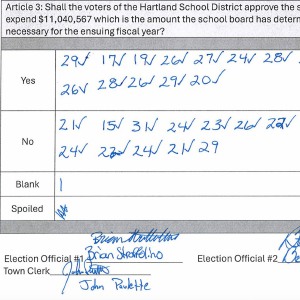 Hartland voters successfully petition for school budget revote
Hartland voters successfully petition for school budget revote
 JAG Productions announces closure, citing ‘crisis facing the arts’
JAG Productions announces closure, citing ‘crisis facing the arts’
 Hanover’s Perreard may soon capture the attention of collegiate coaches in two athletic pursuits
Hanover’s Perreard may soon capture the attention of collegiate coaches in two athletic pursuits
Based on the state inspections, CMS’ certification and enforcement branch has determined that Hanover Terrace is eligible to exit the special focus list, and the notification will come from the state, said regional spokesman Aaron Smith.
State officials will support that change in status, Leon said.
A Key Service
Their purchases of Brookside and Hanover Terrace made their respective new owners important health care providers in this region. Each of the new owners controls one of the three large skilled nursing facilities and about a third of the nursing home bed capacity within a 10-mile radius of Dartmouth-Hitchcock Medical Center.
The third large facility near DHMC is Genesis Lebanon, a 110-bed facility that has a five-star rating and is owned by Genesis Healthcare, the largest nursing home operator in both New Hampshire and Vermont. Genesis operates more than 500 nursing homes and other health facilities nationally. Chesley was the administrator at Genesis Lebanon before taking the top job at Hanover Terrace.
Nursing homes provide critical services to people who require high-level care around the clock. Operators and employees must address the needs of multiple individuals with different health problems and behavioral challenges. Even when resources are abundant — and, in an industry that depends for revenue on the low-paying Medicaid programs, they rarely are — errors and shortcomings can be difficult to avoid.
Meanwhile, residents are vulnerable. Some receive short-term rehabilitation care paid for by Medicare. Others are in for the long term, with chronic or terminal diseases or cognitive disorders. Medicaid pays for many of these residents.
So the conditions and quality of care, and indications that care is getting worse or improving, matter a lot to residents, to their families and friends and to the communities where these facilities operate.
Worsening Conditions At Brookside
Ruth Hebert is 64 years old and, because she requires care for debilitating health problems, has lived at Brookside since August 2014.
Hebert’s father lived at Brookside for 11 years prior to his death in June 2014. “He loved it here,” she said.
Brookside, which had been owned by the same family for five decades, had a five-star rating when, in August 2015, Vermont’s Green Mountain Care Board voted to approve its sale. The buyers, a group of four individuals from New York City, had interests in real estate, development, a home care agency and nursing homes. Some of those homes had one- or two-star ratings.
The new owners borrowed $6 million from the U.S. Housing and Urban Development Department and paid $8 million to acquire Brookside and Green Mountain Nursing and Rehabilitation, a 73-bed facility located 94 miles away in Colchester.
Eli Skaist, the managing member of Brookside’s ownership group, and Mayer Spilman, his assistant, did not respond to requests for comment. Shmuel Love, a member of the group, referred questions about Brookside to local managers including the administrator.
Abraham Rubin, a member of the group that was approved to purchase Brookside, said that he was “not part of the operation” of the facility and declined to say whether he still had an ownership stake. Rubin is not listed as an owner by CMS.
The first serious problem that arose under the new owners, according to Hebert, was the “horrible food.” Although the food has since gotten better, she said, other problems have surfaced and persisted.
Bills have gone unpaid, resulting at least twice in the shutoffs of the residents’ telephone service, according to Hebert. On at least one occasion, uncollected trash piled up outside. Staffing levels have fallen so that, according to Hebert, on some nights only three caregivers are responsible for more than 50 residents. And there have been paycheck miscalculations that have cost employees money and benefits, according to a pending lawsuit.
While the state ombudsmen don’t currently have an individual client who has an open complaint against Brookside, Avildsen said, they are aware that there have been significant problems and a number of residents have been in touch “informally” about staffing and care quality problems.
Brookside’s fall to its current two-star overall rating resulted from health inspections that left it with only one star in that category. Star ratings are primarily based on the results of health inspections by state officials, but also reflect adjustments for staffing numbers and health care services and outcomes reported by facilities.
An Aug. 23 visit in response to a complaint determined that earlier in the month several nurses involved in caring for a patient had mistakenly administered five extra doses of Lasix, a drug used to treat fluid retention.
A more extensive inspection conducted in July as part of Brookside’s license renewal process found multiple deficiencies including, according to the inspection report:
Two mentally impaired residents didn’t receive incontinence care or proper treatment for pressure sores. An inspector observed one of the residents sitting for two hours and 15 minutes without a staff member asking about their need to use the toilet.
A reduction to two, from three, in the number of licensed nursing assistants scheduled to work in a unit that usually had 19 to 21 residents. In addition, some shift overlaps that had helped staff address incontinence and pressure ulcer issues were eliminated.
A failure by caregivers to properly check the insertion of a feeding tube and revise prescriptions for a patient who was unable to safely take food and medication orally.
A failure by caregivers to remove a 3-inch bed bracket that posed an injury hazard to a resident with a history of rolling out of bed.
A failure to screen and develop specialized treatment plans for three patients with mental illness and to give two patients an obligatory written notice that their beds would be held for them during their hospital stays.
An infection threat posed when a licensed nursing assistant neglected to wash hands prior to handling food.
Dirt, grime, dead bugs and food spills on piping, light fixtures, a fan and the floor and ceiling.
Jennifer Combs-Wilber, Brookside’s administrator, signed a plan of correction after that inspection, noting that her signature did not “constitute an admission or agreement by the Provider as to the truth or accuracy of the facts alleged or the conclusions set forth” in the inspection report. She signed a corrective action plan with a similar qualifier after the August inspection.
She declined to be interviewed.
State inspectors also visited Brookside in November and this month, according to Suzanne Leavitt, director of Vermont’s Division of Licensing and Protection, the agency that conducts health inspections at nursing homes. Neither visit found serious violations, she said.
Hands-Off Ownership
The Green Mountain Care Board voted to approve the sale of Brookside and its sister facility after Skaist, the group’s managing member, said in a hearing that he could “almost guarantee I will be there weekly” to oversee operations.
But Hebert said that Skaist rarely visits, and that he and those who have accompanied him on those visits have been unfriendly. “When they come in they speak to no one,” she said. “They are rude to people who say hello.”
“No one here has a good experience of them,” Hebert added.
In July, the new owners reported to the board that they intended “to make a formal request … to allow (Mayer) Spilman to accept all responsibilities currently assigned to Mr. Skaist.”
In November, the owners said they had “not yet made the decision to have Mr. Spilman exclusively manage those responsibilities assigned to Mr. Skaist.”
Skaist, who was listed as a 10 percent owner in the group’s application, also told the board that the new owners would hire a new administrator to replace Thomas Rice, Brookside’s former owner and administrator, who was retiring.
But instead of hiring a new administrator, the new owners added administration duties at Brookside to the duties of Combs-Wilber who was already the administrator of their Colchester facility.
During deliberations on the new owners’ application, members of the Green Mountain Care Board noted the low ratings at other nursing homes controlled by members of the new ownership group.
A Bronx nursing home where Skaist was the administrator rose from two stars to three stars during his tenure, and then back to two stars after he left, they noted. A Michigan nursing home in which two of Brookside’s owners had stakes had only one star, the board members said.
The board then added, as a condition for its approval of the sale, a requirement that the new owners file three so-called implementation reports at six-month intervals during the first 18 months of their tenure.
The second and most recent submission, dated Nov. 3, says that room renovations have begun at Brookside, a boiler system has been repaired and the phone system has been upgraded, and that there have been “no material changes in the services, staffing, operations, organizational structure or bed capacity of the facility.”
However, that filing lists Brookside as a four-star facility as of October 2016, and does not reflect its current two-star rating.
Avildsen said the ombudsman unit, which sends a staffer to each Vermont nursing home each quarter, is planning to send two staffers to visit Brookside: “The staff is aware that there are complaints and we are taking them seriously.”
Other problems have surfaced. In August, Terry-Ann Maxwell, a 30-year employee, filed a lawsuit in Windsor Superior Court alleging that she was fired illegally by Brookside’s current owners after she complained about errors in employees’ paychecks and threatened to seek help from a lawyer.
The lawsuit alleges that the new owners failed to properly pay and account for wages and deductions in the paychecks of Maxwell, a licensed practical nurse, and others among the home’s 65 employees. At one point, the owners let the employees’ group dental insurance policy lapse but continued deducting premiums from their paychecks, the lawsuit says.
Beth Rattigan, a member of Brookside’s legal team, said the nursing home “denies the allegations in Ms. Maxwell’s complaint in their entirety.”
Maxwell worked at Brookside from 1986 until she was fired on July 26, according to the lawsuit. Since the new owners took over in October 2015, Maxwell worked as an licensed practial nurse, charge nurse and unit coordinator, according to her lawsuit.
In October, Brookside moved to dismiss Maxwell’s claim that her firing violated a public policy, while Maxwell’s lawyer, Ned Whittington of Hanover, moved for a default judgment upholding her claims that her firing violated the state’s whistleblower and wages laws.
Judge Robert Gerety has not ruled on those motions.
Staffing Solutions, a Woodstock company that provides nurses for temporary assignments at local health care facilities, also ran out of patience with the new owners, according to co-founder and staffing director Kelly Smithson.
Staffing Solutions says it repeatedly failed to collect unpaid bills from Brookside and stopped sending nurses there in November. It was difficult step for the company to take, Smithson said. The company had been providing services to Brookside since 2004, she said: “You don’t want to not be there to help them.”
On Dec. 21, Staffing Solutions filed its own lawsuit in the Windsor court, alleging that Brookside had violated a contract signed five months earlier and owed $60,600 for nursing services.
The staffing firm also asked for an injunction forbidding Brookside from poaching Staffing Solutions’ employees.
That case closed on Jan. 23, after a Brookside representative named Oded Dashiff signed a stipulation to dismiss that entailed making three installment payments totaling $61,700 to Staffing Solutions, according to court records.
With the ownership change completed, Brookside no longer faces ongoing reviews by the Green Mountain Care Board. Instead, the state’s oversight of the facility will mostly come in relicensing inspections at intervals ranging from nine to 15 months as well as additional inspections triggered by complaints.
Hanover Terrace
Look up Hanover Terrace on Medicare’s rating website (www.medicare.gov/nursinghomecompare/search.html) and an icon appears marking the nursing home, a 39,000-square-foot brick building across Lyme Road from Hanover’s main police and fire station, as a special focus facility — indicating a history of serious problems.
Those problems arose while Hanover Terrace went “through ownership changes and some challenges,” said Chesley, a veteran nursing home administrator who took the reins there in July.
Since then, she said, “a lot of positive changes have occurred.”
Last week, workers and building materials were already visible inside the 47-year-old facility. The new owners plan to spend $300,000 to $400,000 on renovations, Chesley added.
Hanover Terrace was purchased in May by a group led by Jonathan Bleier, who in a 2015 application filed with New York regulators identified himself as the chief financial officer of a 200-bed nursing home in Great Neck, N.Y. Bleier has ownership stakes in another 20 nursing homes, including 11 in Massachusetts, five in Pennsylvania, three in New York and one in Florida, according to a database on the CMS website.
Until June 2014, Hanover Terrace was owned by Kindred Healthcare Inc., a large for-profit company based in Louisville, Ky.
Kindred sold Hanover Terrace to a group made up of CH-Hanover, a limited liability company registered in Delaware, and Chestnut Health and Rehabilitation Group, a corporation that had registered with the Internal Revenue Service as a nonprofit in 2013 but sometimes failed to file the mandatory annual tax returns.
After a short tenure as owners, Chestnut Health and CH-Hanover sold the property to a company controlled by Bleier. Ownership is now divided among Bleier and two trusts, according to CMS. In July, Bleier hired Chesley.
Signs of change include the absence of the locked doors that once separated Hanover Terrace’s front entrance and waiting room from the residential areas and administrative offices.
New cabinets and closets have been installed in residents’ rooms, Chesley said. Kitchen and dining areas are being renovated to support restaurant-style service. And, she said, occupancy has risen from about 70 percent to about 90 percent.
Hanover Terrace also showed significant improvement in its most recent inspections, with no deficiencies that actually harmed or showed systemic potential for harm to residents, according to CMS. A facility must avoid such problems for two inspection cycles to get off the list. An inspection cycle lasts from nine to 15 months.
Still, a relicensing inspection conducted last summer identified five areas in which Hanover Terrace was deficient — although none of them apparently was serious enough to imperil its removal from the special focus list.
Hanover Terrace had failed to develop individualized care plans for 16 of 18 patients surveyed and had failed to properly document hospice visits for two of 18 patients, according to a report dated July 20.
The inspectors also found that over a four-month period Hanover Terrace was lax in its infection control efforts, including numerous instances where patients began treatments with antibiotics without first confirming which pathogen was being treated.
In two instances, caregivers failed to take corrective action after glucometers seemed not to be functioning with acceptable ranges, the inspectors found.
The inspectors also found intravenous and blood draw implements in an unlocked storage area in the nursing home’s area for care for patients with dementia.
Recent inspections that showed no serious deficiencies cleared the way for the removal on the special focus designation. Chesley promised that the push to improve conditions and quality won’t end soon: “We will one day be a five-star building.”
Rick Jurgens can be reached at rjurgens@vnews.com or 603-727-3229.

 Over Easy: ‘A breakfast without a newspaper is a horse without a saddle’
Over Easy: ‘A breakfast without a newspaper is a horse without a saddle’ Lawsuit accuses Norwich University, former president of creating hostile environment, sex-based discrimination
Lawsuit accuses Norwich University, former president of creating hostile environment, sex-based discrimination In divided decision, Senate committee votes to recommend Zoie Saunders as education secretary
In divided decision, Senate committee votes to recommend Zoie Saunders as education secretary
