Former D-H Doctor Who Diverted Pain Drugs Has License Reinstated
| Published: 08-30-2017 1:45 PM |
Lebanon
Dr. Christopher Manfred in January admitted to diverting “a few vials” of hydromorphone, a semi-synthetic opioid derived from morphine, for his personal use and altering patient records to hide his actions, according to a January agreement with the New Hampshire Board of Medicine.
In January, he agreed to voluntarily stop practicing medicine while he began treatment.
In an order issued on Aug. 7, the board permitted Manfred to resume practicing medicine with conditions, including continuing to work with the New Hampshire Professionals Health Program, a nonprofit organization in Amherst, N.H., that oversees treatment and arranges drug testing for physicians, physicians’ assistants, dentists, pharmacists and veterinarians.
“With appropriate treatment and monitoring, the NHPHP routinely helps providers return to work safely,” Manfred’s attorney, Cinde Warmington of the Concord firm of Shaheen and Gordon, wrote in an emailed statement. “Dr. Manfred is grateful for the availability of this program which will assist him as he resumes his practice.”
It was not immediately clear where Manfred, who graduated from the University of New Jersey medical school in 2008 and completed a residency at Dartmouth-Hitchcock Medical Center in 2010, will work.
Manfred is no longer an employee at Dartmouth-Hitchcock, according to D-H spokesman Michael Barwell.
Manfred declined comment on Tuesday.
Article continues after...
Yesterday's Most Read Articles
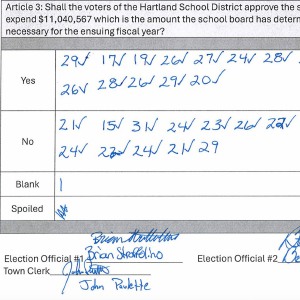 Hartland voters successfully petition for school budget revote
Hartland voters successfully petition for school budget revote
 JAG Productions announces closure, citing ‘crisis facing the arts’
JAG Productions announces closure, citing ‘crisis facing the arts’
 Hanover’s Perreard may soon capture the attention of collegiate coaches in two athletic pursuits
Hanover’s Perreard may soon capture the attention of collegiate coaches in two athletic pursuits
The board’s conditional approval for Manfred’s return to practice requires that for the first year, he only practice critical care medicine.
After the first year, he will need to be reevaluated by Caron Treatment Centers — a substance abuse treatment provider with locations in Pennsylvania and Florida — before resuming work in other areas of medicine, including anesthesiology.
In addition, Manfred will be supervised by a board-approved workplace monitoring physician, who will be responsible for filing quarterly reports with the board about Manfred’s clinical care, conduct and professionalism.
The board’s order requires that Manfred comply with his NHPHP monitoring contract for five years from when he signed it in April or five years following a relapse, should he have one.
The board’s order became final when Manfred agreed to it on Aug. 10, said Penny Taylor, the board’s administrator.
The initial allegations against Manfred came after a routine audit by managers of DHMC’s pharmacy found a “statistically higher utilization of hydromorphone” by a doctor who was later identified as Manfred, according to a board order in January.
Since January, Manfred has complied with the board’s requirements. In addition to seeking treatment, voluntarily ceasing to practice medicine and working with NHPHP, Manfred received approval from Sally Garhart, NHPHP’s program director, to return to practicing in critical care medicine in July and received the board’s approval on Aug. 7, according to an order published on the board’s website earlier this month.
Based on filings provided to the board, it determined that “it is safe for him to commence practicing medicine in a critical care setting,” according to the order.
Manfred is one of about 50 physicians, dentists, pharmacists and veterinarians whose recovery NHPHP is responsible for monitoring, Garhart said.
Despite the opioid epidemic, the clinicians NHPHP monitors primarily struggle with alcoholism, not addictions to other substances, she said.
“It’s legal and it’s available ... and then people get into trouble,” she said.
Garhart emphasized that recovery is possible and that five years of monitoring “helps people make a strong commitment” to maintaining their sobriety.
It’s “really important to give people hope,” she said.
Just because someone is struggling with addiction “doesn’t mean that they’re an awful person (and it) doesn’t mean that they can’t turn their life around,” she said.
Nora Doyle-Burr can be reached at ndoyleburr@vnews.com or 603-727-3213.

 At Dartmouth, hundreds protest ongoing war in Gaza and express support for academic freedom
At Dartmouth, hundreds protest ongoing war in Gaza and express support for academic freedom Over Easy: ‘A breakfast without a newspaper is a horse without a saddle’
Over Easy: ‘A breakfast without a newspaper is a horse without a saddle’
